The following is an article from The Annals of Improbable Research.
 (Image credit: Flickr user Flavia)
(Image credit: Flickr user Flavia)
by Paul Mackin, MB BS PhD MRCPsych
Peter Gallagher, BSc (Hons) MPhil
Lucy Robinson, BSc (Hons)
School of Neurology Neurobiology and Psychiatry, Department of Psychiatry
University of Newcastle upon Tyne
Newcastle upon Tyne, U.K.
A recently published hypothesis proposes that, in country after country, the prevalence of schizophrenia increased following the introduction of heeled footwear. That hypothesis does not account for differing footwear styles. In this report, we attempt to remedy that lack.
We examine the risk of schizophrenia in individuals wearing stiletto heels.
Flensmark’s High Hypothesis
Is there an association between the use of heeled footwear and schizophrenia? This is the question posed in a recent paper by Jarl Flensmark, published in the journal Medical Hypotheses.1 Flensmark’s article highlights that the increase use and availability of heeled footwear has been paralleled by an increase in the prevalence of schizophrenia.
Flensmark presents a cogent argument supported by historical and epidemiological data together with a possible pathophysiological mechanism to account for the phenomenon.
The mechanism underlying this phenomenon, Flensmark suggests, is obvious. Heeled footwear, he explains, reduces stimulation of mechanoreceptors in the lower extremities which would normally increase activity in cerebello-thalamo-cortico-cerebellar loops through their action on NMDA receptors, and that this reduction in cortical activity changes dopaminergic function which involves the basal ganglia-thalamo-cortical-nigro-basal ganglia loops.
If Flensmark is correct, there are far-reaching consequences for the prevention and treatment of mental illnesses. The role of drugs in the management of these disorders is controversial, and the Flensmark hypothesis casts a dark shadow over the future of psychopharmacology.
This argument would have been further strengthened, however, by considering the relationship between the prevalence of schizophrenia and individual footwear styles. We offer some thoughts about the deleterious effects upon mental health of stiletto shoes, and conclude with a simple intervention which, based on Flensmark’s observations, may offer therapeutic benefit to both the mental and physical health of those suffering from schizophrenia.
If this pathophysiological mechanism is correct one would expect to observe a higher prevalence of schizophrenia in individuals who wear stiletto heels as high heels increase mechanical loading on the medial forefoot at the expense of other plantar regions,2 and cause changes in postural muscle tone,3 and therefore altered mechanoreceptor stimulation. We undertook a systematic literature search to identify epidemiological and demographic data regarding the risk of schizophrenia in individuals who wear stiletto heels.
 Figure 1. Measuring a stiletto heel (metric). (Image credit: A.S. Kaswell, AIR)
Figure 1. Measuring a stiletto heel (metric). (Image credit: A.S. Kaswell, AIR)
Stilettos and Schizophrenia: Method
We did a systematic walkthrough of the medical literature, looking for reports that involve the two words “stiletto” and “schizophrenia.” We found nothing. We then searched for medical papers that report the average heel size as a function of age. We found some. We then correlated this data with age of hospitalization for schizophrenia.
Schizophrenia and Stilettos: Results
The relationship between hospitalizations for schizophrenia and average heel height is represented graphically in figure 3. [Ed. note: which is unavailable.]
Stiletto heels are rarely worn before the age of fifteen, and schizophrenic illnesses are rarely diagnosed before this age. Heel height increases sharply, however, over the subsequent three years, closely mirroring the sharp increase in the incidence of schizophrenia. The mean age for the first wearing of heels 1, 2 and 3 inches high is 15.1, 16.7 and 18.5 years, respectively.4 The wearing of stiletto heels decreases throughout adulthood as does the heel height. It is of particular interest to note that the maximum heel height corresponds to the peak hospitalization rate, and as heel height decreases so too does hospitalization.
Stilettos and Schizophrenia: Discussion
High heels are worn most frequently, but not exclusively, by females. We are not aware of any data regarding the average height of the heel size of men’s footwear, or how this may change over time. This is clearly an area worthy of further research.
Preliminary data do suggest, however, that male cross-dressers may have a higher rate of schizophrenia,5 although we are careful to emphasize that it is not clear that all male cross-dressers wear stiletto heels, some perhaps preferring a simple flat shoe or an open-toe sandal.
The possible relationship between plantar mechanoreceptor stimulation and schizophrenia raises interesting questions regarding therapeutic intervention. Should Flensmark’s hypothesis be true, increasing plantar mechanoreceptor stimulation should offer protection from developing a psychotic illness to vulnerable individuals (e.g. those with high genetic loading), as well as improving the illness course of those with an established schizophrenic illness.
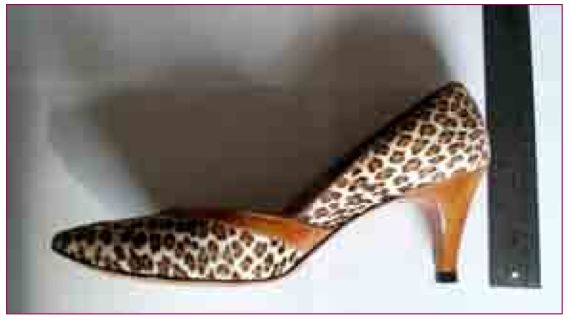 Figure 2. Measuring a stiletto heel (non-metric). By tradition, this method of measurement is the preferred one. (Image credit: A.S. Kaswell, AIR)
Figure 2. Measuring a stiletto heel (non-metric). By tradition, this method of measurement is the preferred one. (Image credit: A.S. Kaswell, AIR)
Steps for Treatment
We propose a simple and highly cost-effective intervention which simply involves repetitive forceful stepping on the spot, twice daily (Step-b.d). This program of activity could be easily incorporated into the daily routine and would obviate the need for regular contact with physicians to monitor compliance or side effects, although we would advocate a six-monthly check-up with a state registered chiropodist.
[We would not wish this to be confused with the highly successful Systematic Treatment Enhancement Program for Bipolar Disorder (STEPBD), which is currently running in the USA, and, accordingly, we propose the Schizophrenia Kinetic Intervention for Prophylaxis (SKIP-BD)].
Apart from the potential therapeutic benefit on schizophrenic symptoms, there are also other clear benefits associated with this intervention. Patients with schizophrenia are at a higher risk of developing osteoporosis,6 and there is clear data to suggest that jumping up and down on the spot prevents bone loss and osteoporosis.7 Furthermore, the increased aerobic exercise would offer protection against cardiovascular disease, obesity and diabetes, which are more prevalent in patients with schizophrenia.8
Controlled trials of the SKIP-BD program are urgently needed, as a positive outcome would have dramatic resource implications for all developed healthcare systems, as well as for the pharmaceutical industry. The need for costly Early Intervention in Psychosis programs would be abolished, and the costs associated with antipsychotic drug prescriptions would be decimated. Pending the results of these trials, we strongly recommend that patients continue to take prescribed medication. Patients and doctors, of either sex, should wear the stiletto heel at their peril.
Conflict of Interests
PM and PG have no personal experience of wearing footwear with heel heights exceeding one inch. There are no other conflicts of interest that will be mentioned here.
References
1. “Is There an Association Between the Use of Heeled Footwear and Schizophrenia?” J. Flensmark, Medical Hypotheses, vol. 63, 2004, pp. 740-47
2. “The Effects of Wearing High Heeled Shoes on Pedal Pressure in Women,” R.E. Snow and K.R. Williams, Foot and Ankle, vol. 13, 1992, pp. 85-92.
3. “Postural Alignment in Barefoot and High-Heeled Stance,” K.A. Opila, et al.,
Spine, vol. 13, 1988, pp. 542-47.
4. The Prevalence of Foot Problems in Older Women: A Cause for Concern,” J. Dawson, et al., Journal of Public Health Medicine, vol. 24, 2002, pp. 77-84.
5. “A Comparison of Treated and Untreated Male Cross-Dressers,” J.L. Croughan, et al., Archives of Sexual Behavior, vol. 10, 1981, pp. 515-28.
6. “Schizophrenia and Osteoporosis,” M. Lean and G. De Smedt, International Clinical Psychopharmacology, vol. 19, 2004;, pp. 31-35.
7. “Long-Term Exercise Using Weighted Vests Prevents Hip Bone Loss in Postmenopausal Women,” C.M. Snow, et al., Journals of Gerontology. Series A, Biological Sciences and Medical Sciences, vol. 55, 2000, pp. M489-91.
8. “Diet, Diabetes and Schizophrenia; Review and Hypothesis,” M. Peet, British Journal of Psychiatry, vol. 184, suppl. 47, 2004, pp. S102-105.
[EDITOR’S NOTE: For a detailed look at the Flensmark hypothesis, see “Trouble Underfoot” in AIR, vol. 11, no. 1, January-February 2005.]
_____________________
 This article is republished with permission from the March-April 2005 issue of the Annals of Improbable Research. You can download or purchase back issues of the magazine, or subscribe to receive future issues. Or get a subscription for someone as a gift!
This article is republished with permission from the March-April 2005 issue of the Annals of Improbable Research. You can download or purchase back issues of the magazine, or subscribe to receive future issues. Or get a subscription for someone as a gift!
Visit their website for more research that makes people LAUGH and then THINK.





9(MDAzNTYzNDk2MDEyNDM5NTU1OTc1NDZmZQ001))
 Fortunately, we’ve come a long way since the theory that less-than-affectionate mothers cause
Fortunately, we’ve come a long way since the theory that less-than-affectionate mothers cause  The causes of
The causes of 
 (Image credit: Flickr user
(Image credit: Flickr user  Figure 1. Measuring a stiletto heel (metric). (Image credit: A.S. Kaswell, AIR)
Figure 1. Measuring a stiletto heel (metric). (Image credit: A.S. Kaswell, AIR)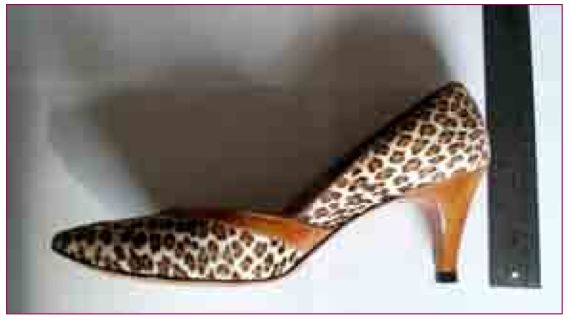 Figure 2. Measuring a stiletto heel (non-metric). By tradition, this method of measurement is the preferred one. (Image credit: A.S. Kaswell, AIR)
Figure 2. Measuring a stiletto heel (non-metric). By tradition, this method of measurement is the preferred one. (Image credit: A.S. Kaswell, AIR) This article is republished with permission from the
This article is republished with permission from the  Rare genetic changes that may be responsible for the development of
Rare genetic changes that may be responsible for the development of